OWERVIEW
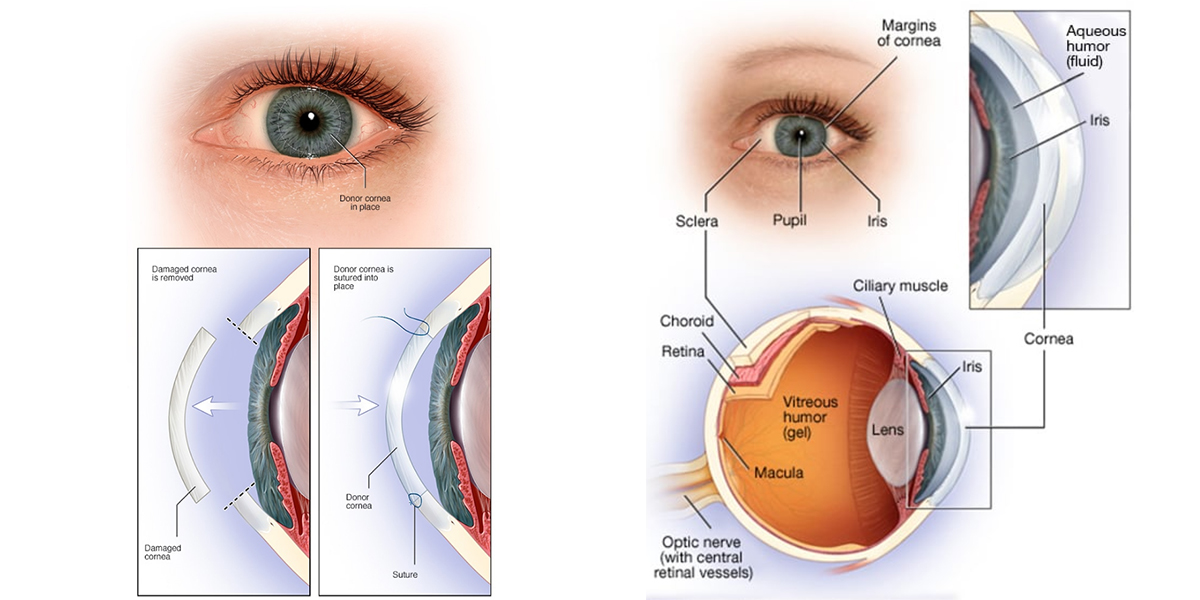
A cornea transplant (keratoplasty) is a surgical procedure to replace part of your cornea with corneal tissue from a donor. Your cornea is the transparent, dome-shaped surface of your eye. It’s where light enters your eye and is a large part of your eye’s ability to see clearly.
A cornea transplant can restore vision, reduce pain, and improve the appearance of a damaged or diseased cornea.
Most cornea transplant procedures are successful. But cornea transplant carries a small risk of complications, such as rejection of the donor cornea.
Why it’s done
A cornea transplant is most often used to restore vision to a person with a damaged cornea. A cornea transplant can also relieve pain or other signs and symptoms associated with cornea diseases.
A number of conditions can be treated with a cornea transplant, including:
- A cornea that bulges outward (keratoconus)
- Fuchs’ dystrophy, a hereditary condition
- Thinning or tearing of the cornea
- Cornea scarring, caused by infection or injury
- Swelling of the cornea
- Corneal ulcers not responding to medical treatment
- Complications caused by previous eye surgery
Risks
Cornea transplant is relatively safe. Still, it does carry a small risk of serious complications, such as:
- Eye infection
- Pressure increase within the eyeball (glaucoma)
- Problems with the stitches used to secure the donor cornea
- Rejection of the donor cornea
- Bleeding
- Retinal problems, such as retinal detachment or swelling
Signs and symptoms of cornea rejection
Your body’s immune system can mistakenly attack the donor cornea. This is called rejection, and it might require medical treatment or another cornea transplant.
Make an urgent appointment with your eye doctor if you notice signs and symptoms of rejection, such as:
- Loss of vision
- Eye pain
- Red eyes
- Sensitivity to light
Rejection occurs in about 10% of cornea transplants.
How you prepare
Before cornea transplant surgery, you will undergo:
- A thorough eye exam. Your eye doctor looks for conditions that might cause complications after surgery.
- Measurements of your eye. Your eye doctor determines what size donor cornea you need.
- A review of all medications and supplements you’re taking. You may need to stop taking certain medications or supplements before or after your cornea transplant.
- Treatment for other eye problems. Unrelated eye problems, such as infection or inflammation, can reduce your chances of a successful cornea transplant. Your eye doctor will treat those problems before your surgery.
Finding a donor cornea
Corneas used in cornea transplants come from people who have died. Corneas are not used from people who died from unknown causes or from donors who had certain conditions, such as diseases that can spread, previous eye surgery or eye disease.
Unlike with organs such as livers and kidneys, people needing cornea transplants don’t require tissue matching. In the United States, donor corneas are widely available so there’s usually not a long waiting list.
Procedures to transplant a portion of the cornea
A cornea transplant removes either the entire thickness or partial thickness of the diseased cornea and replaces it with healthy donor tissue. Your cornea surgeon will decide which method to use. These types of procedures include:
- Penetrating keratoplasty (PK) a full-thickness cornea transplant. Your surgeon cuts through the entire thickness of the abnormal or diseased cornea to remove a small button-sized disk of corneal tissue. A special instrument is used to make this precise circular cut.
The donor cornea, cut to fit, is placed in the opening. Your surgeon then uses stitches (sutures) to stitch the new cornea into place. The stitches might be removed at a later visit with your eye doctor.
- Endothelial keratoplasty (EK). These procedures remove diseased tissue from the back corneal layers, including the endothelium and a thin layer of tissue that protects the endothelium from injury and infection (Descemet membrane). Donor tissue replaces the removed tissue.
There are two types of endothelial keratoplasty. The first type, called Descemet stripping endothelial keratoplasty (DSEK), uses donor tissue to replace about one-third of the cornea.
The second type, called Descemet membrane endothelial keratoplasty (DMEK), uses a much thinner layer of donor tissue. The tissue used in DMEK is extremely thin and fragile. This procedure is more challenging than DSEK and is commonly used.
- Anterior lamellar keratoplasty (ALK). Two different methods remove diseased tissue from the front corneal layers, including the epithelium and the stroma, but leave the back endothelial layer in place.
The depth of cornea damage determines the type of ALK procedure that’s right for you. Superficial anterior lamellar keratoplasty (SALK) replaces only the front layers of your cornea, leaving the healthy stroma and endothelium intact. A deep anterior lamellar transplant (DALK) procedure is used when cornea damage extends deeper into the stroma. Healthy tissue from a donor is then attached (grafted) to replace the removed portion.
- Artificial cornea transplant (keratoprosthesis). In some cases, if people aren’t eligible for a cornea transplant from a donor cornea, they might receive an artificial cornea (keratoprosthesis).
Your doctor will discuss which method of corneal transplant surgery is best for you, what to expect during the procedure and explain the risks of the procedure.
What you can expect
During the procedure
On the day of your cornea transplant, you’ll either be given a sedative to help you relax and a local anesthetic to numb your eye, or you’ll be put to sleep. Either way, you shouldn’t feel pain.
Surgery is done on one eye at a time. The amount of time spent in surgery is different and depends on your situation.
After the procedure
Once your cornea transplant is completed, you can expect to:
- Receive medications. Eyedrops and, sometimes, oral medications immediately after cornea transplant and during recovery will help control infection, swelling and pain. Eyedrops to suppress the immune system help prevent cornea rejections.
- Wear eye protection. Eye shields or glasses protect your eye as it heals.
- Lie on your back. Depending on the type of transplant, you might have to do this for a while after surgery to help the new tissue stay in place.
- Avoid injury. Plan to take it easy after your cornea transplant, and slowly work your way up to your normal activities, including exercise. Don’t rub or press on your eye. For the rest of your life, you’ll need to take extra precautions to avoid harming your eye.
- Return for frequent follow-up exams. Expect to see your eye doctor regularly in the year after surgery to monitor your progress and look for complications.
Results
Most people who receive a cornea transplant will have their vision at least partially restored. What you can expect after your cornea transplant depends on the reason for your surgery and your health.
Your risk of complications and cornea rejection continues for years after your cornea transplant. For this reason, see your eye doctor annually. Cornea rejection can often be managed with medications.
Vision correction after surgery
Your vision might initially be worse than before your surgery as your eye adjusts to the new cornea. It can take several months for your vision to improve.
Once the outer layer of your cornea has healed — several weeks to several months after surgery — your eye doctor will work to make adjustments that can improve your vision, such as:
- Correcting unevenness in your cornea (astigmatism). The stitches that hold the donor cornea in place on your eye might cause dips and bumps in your cornea, making your vision blurry in spots. Your doctor might correct some of this by releasing some stitches and tightening others.
- Correcting vision problems. Refractive errors, such as nearsightedness and farsightedness, can be corrected with glasses, contact lenses or, in some cases, laser eye surgery.

 English
English Français
Français Deutsch
Deutsch العربية
العربية